COVID-19 and The Road Ahead

From Boosters & Breakthroughs to Vaccines & Variants: Where Do We Go From Here?
The following reflects an 8/24/2021 discussion; please check the CDC website for real-time updates as the situation continues to evolve.
Their answers may not land lightly, but epidemiologist Jodie Guest, PhD, and drug development expert Michael Kinch, PhD, have been immersed in examining COVID-19 since its first stirrings in early 2020. They share an informed look at the road ahead for us all.
State of Concern
Noting more than 39 million COVID-19 cases nationwide, (as of 9/2/21) Guest projects this will continue to rise rapidly and eclipse one million a week. While “hot spots” for outbreaks clearly correspond to the country’s most lightly vaccinated locales, the impact of the delta variant is being felt in virtually every state. “There’s almost nowhere you can go in the U.S. that you don’t need to be masked indoors, even if vaccinated,” she says. The progressive increase in vaccinated patients with COVID-19 in European hospitals is also troubling, says Kinch, a potential harbinger of what is to come for the U.S.
However, what’s driving the surge is not cases among the vaccinated, known as “breakthroughs.” It’s a term Guest would like to eliminate permanently, given its negative connotation regarding vaccine efficacy. “These type of infections are still rare. More than 90% of those hospitalized with COVID-19 are unvaccinated.” She points out that while viral loads in patients with COVID-19 are the same for vaccinated and unvaccinated patients in the first few days of illness, they drop much faster and further in the vaccinated.
The vaccine, contends Kinch, was never intended to eliminate all possibility of getting COVID-19. “It’s not a suit of armor,” he says, “because no vaccine ever provides 100% protection. But we know they work incredibly well to prevent you from getting very sick or dying.”
The FDA’s recent approval of the Pfizer mRNA vaccine, with Moderna approval expected to follow soon, is pivotal, says Guest, in helping launch vaccination requirements at businesses, schools and other locations. “Don’t underestimate the importance of this approval in providing support for mandates that will protect all of us,” she says. “Recognize that in the entire history of vaccines, there has never been a set more studied than the ones we have now.”
Adds Kinch, “With the enormous amount of data gathered on the vaccines’ efficacy and safety, those who think of themselves as vaccine hesitant may more accurately be described as vaccine resistant.”
Third Doses and Boosters
The recent approval of a third dose of Pfizer or Moderna for immunosuppressed patients who didn’t build sufficient immunity from the first two doses applies to just 3% of the adult population. For everyone else (with the exception of pregnant women), a booster shot six to eight months after the initial series is being considered for approval.
“Right now, that’s how long we believe we can go without significantly diminished immunity,” says Guest. Antibody tests are not proven to be an accurate measure of protection from COVID-19, says Kinch, because the antibody levels vary by individual.
If you received Pfizer or Moderna initially, choose the same for a booster. Notes Kinch: “There’s no difference between these two vaccines—one is not better than the other.” In fact, some studies show no impact on efficacy from switching brands, he says; Johnson & Johnson data is yet to come.
And where does the flu shot fit in this fall? Absolutely essential, both agree, with the only caution that a two-week separation between the two vaccines may be recommended by some healthcare providers to avoid triggering a hyperactive immune response.
Protecting our Children
The best way to keep youngsters under 12 safe is ensuring that everyone around them is vaccinated, says Guest.
“Teachers, caregivers, babysitters and others should be vaccinated, or fully masked whenever they’re with children,” she advises. A different dose is being tested for 5- to 12-year-olds, with approval possible later this year.
The Next Wave of Variants?
While not identified by the Centers for Disease Control (CDC) as a “high concern,” Kinch admits that the lambda variant worries him primarily because not enough is known about its ability to resist vaccines. “One view is that the COVID-19 spike protein can only mutate to a certain point, and if that’s true, lambda could be the end of the virus. The other view is that we don’t know if it stopped mutating,” he says.
“We’re not defenseless, though,” counters Guest, “because we can keep it from getting here by having COVID-19 not circulating in communities. Greater numbers of vaccinated people will prevent us from getting whatever variant might follow delta.”
Stay Safe and Well
One of last year’s most popular signoff lines takes on new resonance as our experts advise on what that now means for the vaccinated in fall 2021.
Mask Up, Indoors and Out.
Masks are increasingly needed outside in crowded areas. Indoors, remember that while a soft, comfortable cloth mask protects others from you, if you need extra protection in certain settings, use a KN95 or N95 mask.
Pass on Indoor Dining, Movies, Concerts and Sporting Events.
Also reconsider full-capacity outdoor events with no masking/distancing/vaccine requirements. (As an alternative, order take-out and support virtual events offered by local venues). And avoid getting together in person with those who are not vaccinated.
Reach out to Every Unvaccinated Person you Know.
“The best action we can take is to keep encouraging every unvaccinated person we know to get the shot, now,” advises Guest. “We’re all in the race against variants and need to work together to defeat them as quickly as possible.” Adds Kinch, “It’s unfortunate that the motivations behind much of the messaging has messed up the message itself. Be completely honest about what is known and not known about the vaccine.”
The Swiss Cheese Respiratory Pandemic Defense.
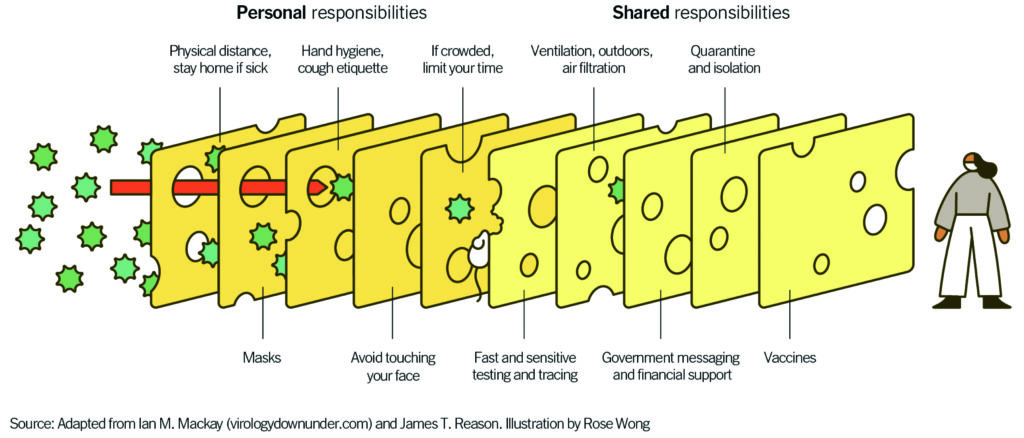 “Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”
“Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”
Dr. Jodie Guest is professor and vice chair of the Department of Epidemiology, Emory University, Atlanta, and award-winning leader of Emory’s Outbreak Response Team for COVID-19.
Dr. Michael Kinch is associate vice chancellor and founder/director of the Center for Research Innovation in Biotechnology and the Center for Drug Discovery at Washington University, St. Louis.
The post COVID-19 and The Road Ahead appeared first on Specialdocs Consultants.
For more information on the benefits of Concierge Medicine, please visit Logan Square Medical Group. To enroll as a new patient, please call us directly at (773) 489-7040a>. Current patients with any health concerns, should call Dr. Brown’s office directly at (773) 489-7040a>. Thank you!