Bone Up: What Is Osteoporosis?
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low bone mass that results in increased risk of bone fracture, sometimes even from a minor fall or pressure from a big hug. Over 1.5 million osteoporotic fractures occur annually, and 1/3 of women and 1/5 of men over 50 will experience an osteoporotic bone fracture in their lifetime. The good news is that reliable diagnostic testing and treatments are available, which we share below.
Who’s at Risk for Osteoporosis?
Osteoporosis is sometimes referred to as a “silent disease” because it is painless unless a fracture occurs, so people often are unaware they have it until that happens. Post-menopausal women are at highest risk, in part due to the decline in estrogen levels. Estrogen, and to an even greater extent, testosterone, are hormones that help ward off osteoporosis, which is why it is not as common in men. Others at risk include those with autoimmune diseases such as rheumatoid arthritis and celiac disease, those with high parathyroid or thyroid levels and certain other chronic diseases.
Medications including corticosteroids, proton pump inhibitors and certain antidepressants and anti-seizure medications may increase risk of bone thinning. Inherited factors may affect risk, such as race (more common in Caucasians and Asians), body shape and size (smaller/thinner individuals more at risk) and family history of osteoporosis. Physical activity level and diet play a role, placing those who are sedentary and/or have a diet low in calcium at higher risk. Cigarette smoking and higher alcohol intake are also risk factors.
How Osteoporosis is Diagnosed
A bone density measurement test is the best way to diagnose osteoporosis, using the DEXA (dual energy x-ray absorptiometry) scan of hip and spine. The severity of decrease in bone mass is determined by your T-score: Between -1.0 and -2.5 is defined as osteopenia, when bones are weaker than normal, while -2.5 or less indicates osteoporosis.
Osteoporosis Medications
A number of medications are available to treat osteoporosis.
- Bisphosphonates to slow the breakdown and removal of bone are typically tried first. Fosamax, used most, is a weekly pill often taken for 5 years followed by a “drug holiday.” The IV bisphosphonate Reclast is generally continued for three years.
- Evista is a daily pill for post-menopausal osteoporosis that protects against bone loss and also reduces the risk of breast cancer in high-risk women.
- Prolia is injected every 6 months to slow breakdown and removal of bone and help increase bone density. It should not be discontinued once started or must be followed by another medication if stopped.
- Evenity is injected once a month for a year to increase new bone and reduce breakdown and removal of bone.
- Forteo and Tymlos are drugs that help build bone for people at high risk of fracture. These are injected daily for two years.
Managing Osteoporosis
Peak bone mass is achieved by age 25-30 years, but at any age, a healthy lifestyle can aid in strengthening bones. Focus on eating a balanced diet rich in vitamin D and calcium (see sidebar), and remember that exposing the body to natural sunlight increases production of vitamin D. Eliminating tobacco use and limiting alcohol is strongly recommended to promote maximum absorption of calcium and vitamin D. Taking fall prevention measures is crucial: consider that 95% of hip fractures are caused by falls.
Aim for 30 minutes of weight-bearing and muscle strengthening exercises on most days:
- Walk or run on level ground or a treadmill
- Dance
- Climb stairs
- Lift weights without straining your back
- Sit-to-stand exercises: start with an elevated seat height, and progress to a lower chair as you get stronger
- Strengthen thighs: stand against a wall and slide down into a slight knee bend, hold for 10 seconds and repeat a few times
- Tai Chi: combines slow movements, breathing exercises, and meditation
Nourishment Know-How for Bone Health
For optimal bone health, a daily intake of 1200-1500 mg of calcium and 400-800 IU (international units) of Vitamin D is recommended for adults. In many cases, supplementation may be appropriate.
Selected sources with calcium and/or Vitamin D:
- Dairy products
- Calcium- and vitamin D-fortified foods and beverages (soy or almond milks, cereals, cheese)
- Dark green, leafy vegetables
- Fish such as salmon, trout, mackerel, tuna, sardines
- Egg yolks
- Sesame or chia seeds, figs, almonds
Fall Prevention Measures for Those with Osteoporosis Include:
- Avoid ladders, step-stools and roof work
- Eliminate tripping hazards like throw rugs, obstacles or cords on the floor
- Be careful around pets and leashes
- Use good lighting, night lights, update glasses and eye care to optimize vision
- Stay fit with regular strengthening and balance exercises
- Wear non-slip shoes
- Install handrails and grab bars in the bathroom
Every patient is unique…please check with your healthcare provider to discuss recommendations for prevention and treatment based on your individual health situation.
Sources: Arthritis Foundation, AAOS, Orthoworld, Cleveland Clinic, National Academy of Medicine (formerly Institute of Medicine), UpToDate, US Department of Agriculture, American College of Rheumatology.



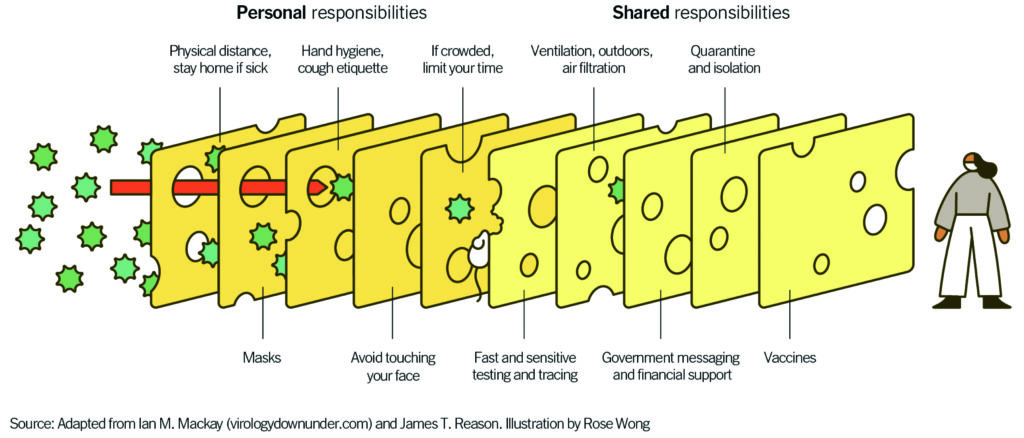 “Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”
“Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”