Ticked Off: How to Recognize, Relieve and Resist Lyme Disease
Summertime is prime time for ticks, which are becoming more prevalent each year. A combination of changing land use and warmer winters has greatly expanded the ticks’ habitat and they’re now found in more than half of U.S. counties. As a result, tick-borne Lyme disease has doubled over the last two decades to nearly 500,000 cases annually, earning it the unfortunate distinction of being the most common vector-borne illness in the Northern hemisphere. Read on for details on how to protect yourself this season, and in the summers to come.
Identifying Lyme
In its acute phase (one to two weeks after the bite), Lyme can cause fevers and chills, joint pain, headache, muscle aches and is frequently accompanied by a salmon-colored rash at the site of the tick bite. It may have a “bulls-eye” appearance, often considered a sign of infection, but the rash can manifest differently, or not at all. Diagnosis is based on symptoms, physical findings (e.g., rash), the possibility of exposure to infected ticks, and antibody tests. A high number of false negative tests occur in the early phase, however, because it takes time for the immune system to respond to the infection and create antibodies. As the infection progresses, virtually everyone with Lyme disease has a positive test result.
Treating early, late and long Lyme
Most people recover from Lyme disease rapidly and completely if diagnosed early and treated with a short course of oral antibiotics. More serious symptoms, including joint pain and swelling, nerve problems and neurological issues, may develop if Lyme disease is left untreated. Known as late Lyme disease, it can occur months to years after a tick bite, and requires a longer course of antibiotics, administered intravenously. Post-Treatment Lyme disease, sometimes called chronic or long Lyme disease, is experienced by 5% to 15% of patients who have lingering symptoms such as headache, fatigue, joint pain and “brain fog.” While the condition is not yet well understood, experts have found additional antibiotic treatments are not usually helpful, and the symptoms gradually resolve over time.
Preventing Lyme
The best way to avert the complications of Lyme disease is to vigilantly avoid ticks. These tips can help you prevent Lyme disease:
- Wear shoes, long pants tucked into socks, a long-sleeved shirt, hat and gloves in wooded or grassy areas.
- Stick to trails, stay clear of low bushes and long grass.
- Use insect repellants such as DEET, picardin, permethrin (apply to clothing).
- Do tick checks on your body after outside activities. Be sure to check your dogs for ticks
too! - Remove any ticks promptly with clean, fine-tipped tweezers. Be reassured that just finding a tick on your skin doesn’t mean you’ll get Lyme disease; a tick needs to be attached for at least 48 hours before it can transmit the bacteria.
- Look for advanced protection in the next few years from two well-known names in vaccines – Pfizer and Moderna. An earlier vaccine, LYMERix, was discontinued in 2002 due to lack of interest at a time of lower Lyme disease cases, as well as concerns over side effects. Pfizer’s VLA15 is intended to block the bacteria from leaving the tick. Moderna is applying mRNA technology used in its COVID vaccine to target the Borrelia bacteria species at the root of most U.S. Lyme disease cases. Also of note is MassBiologics’ shot that delivers a single, human anti-Lyme antibody directly to a person to provide immediate immunity…now in trials.
QUICK BITES: Fast Facts About Lyme Disease
- Most Lyme disease infections in the U.S. occur May through September.
- Cases of Lyme disease are most commonly seen in the northeast and mid-Atlantic states
(from Maine to Virginia), the Midwest (Minnesota, Wisconsin, and Michigan), and the
West Coast (California). - The disease was first recognized in Old Lyme, Connecticut in 1975 when a cluster of
children developed unexplained, rheumatoid arthritis-like symptoms. Not until the next decade was the cause discovered: the spiral bacteria Borrelia burdorferi in deer ticks prevalent in the forests near where the infections occurred. Testing confirmed the Lyme disease bacterium was passed to humans via the bite of a deer tick.
Sources: NIH, National Geographic


 1.
1.  2.
2.  3.
3.  4.
4.  5.
5.  6.
6.  7.
7. 


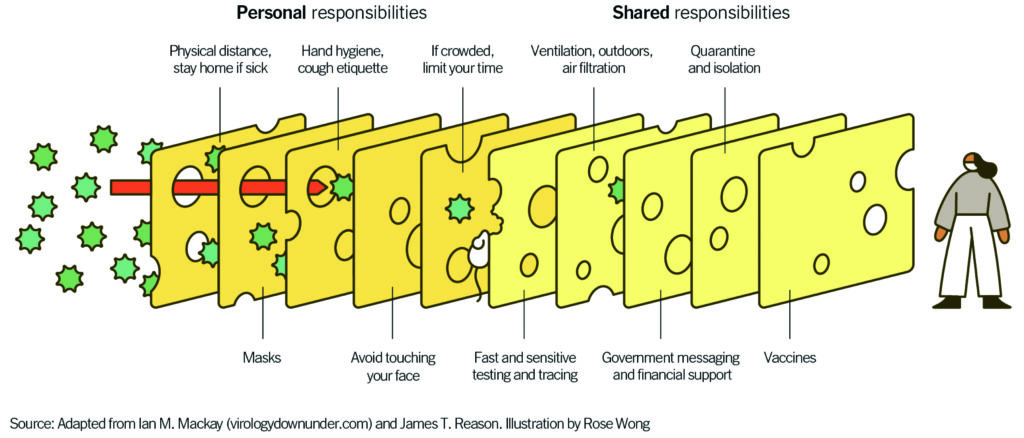 “Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”
“Layering prevention messages is crucial because the delta variant has made the holes in the Swiss cheese slice of the vaccine just a bit bigger,” says Guest. “Now masks are more crucial than ever before.”